What is the partial pressure of oxygen po2. Atmospheric pressure, partial pressure of inhaled O2 (humidified inhaled air) and partial pressure of O2 in alveolar air at various altitudes above sea level. Influence of flight conditions on the organization
(The last column shows the O 2 content, from which the corresponding partial pressure at sea level can be reproduced (100 mm Hg = 13.3 kPa)
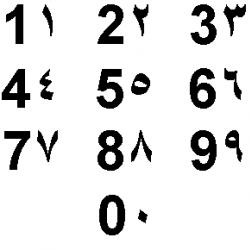
| Height, m | Air pressure, mm Hg Art. | Partial pressure O 2 in the inhaled air, mm Hg. Art. | Partial pressure of O 2 in alveolar air, mm Hg Art. | Equivalent fraction O 2 |
| 0,2095 | ||||
| 0,164 | ||||
| 0,145 | ||||
| 0,127 | ||||
| 0,112 | ||||
| 0,098 | ||||
| 0,085 | ||||
| 0,074 | ||||
| 0,055 | ||||
| 0,029 | ||||
| 0,4 | 0,014 |
Rice. four. Zones of influence of oxygen deficiency when climbing to a height
3. Zone of incomplete compensation (zone of danger). It is implemented at altitudes from 4000 m to 7000 m. Unadapted people develop various disorders. When the safety limit (violation threshold) is exceeded, physical performance drops sharply, the ability to make decisions weakens, and arterial pressure, consciousness gradually weakens; possible muscle twitches. These changes are reversible.
4. Critical zone. Starts from 7000 m and above. P A O 2 gets lower critical threshold - those. its lowest value, at which tissue respiration can still be carried out. According to various authors, the value of this indicator ranges between 27 and 33 mm Hg. Art. (V.B. Malkin, 1979). Potentially lethal disorders of the central nervous system occur in the form of inhibition of the respiratory and vasomotor centers, the development of an unconscious state and convulsions. In the critical zone, the duration of oxygen deficiency is of decisive importance for the preservation of life. fast promotion PO 2 in the inhaled air can prevent death.
Thus, the effect on the body of reduced partial pressure oxygen in the inhaled air under conditions of a drop in barometric pressure is not realized immediately, but upon reaching a certain reaction threshold corresponding to an altitude of about 2000 m. This situation is facilitated by the features of the interaction of oxygen with hemoglobin, which are graphically displayed by the oxyhemoglobin dissociation curve (Fig. 5).
Fig.5. Dissociation curves of oxyhemoglobin (Hb) and oxymyoglobin (Mb)
S-shaped the configuration of this curve, due to one hemoglobin molecule binds four oxygen molecules plays an important role in the transport of oxygen in the blood. In the process of oxygen absorption by the blood, PaO 2 approaches 90-95 mm Hg, at which hemoglobin saturation with oxygen is about 97%. At the same time, since the dissociation curve of oxyhemoglobin in its right part is almost horizontal, with a drop in PaO 2 in the range from 90 to 60 mm Hg. Art. saturation of hemoglobin with oxygen does not decrease much: from 97 to 90%. Thus, due to this feature, a drop in PaO 2 in the indicated range (90-60 mm Hg) will only slightly affect blood oxygen saturation, i.e. on the development of hypoxemia. The latter will increase after overcoming PaO 2 lower limit - 60 mm Hg. Art., when the oxyhemoglobin dissociation curve changes from a horizontal to a vertical position. At an altitude of 2000 m, PaO 2 is 76 mm Hg. Art. (10.1 kPa).
In addition, the drop in PaO 2 and the violation of hemoglobin saturation with oxygen will be partially compensated by increased ventilation, an increase in blood flow velocity, mobilization of deposited blood, and the use of the oxygen reserve of blood.
A feature of hypobaric hypoxic hypoxia, which develops when climbing in the mountains, is not only hypoxemia, but also hypocapnia (a consequence of compensatory hyperventilation of the alveoli). The latter determines the formation gas alkalosis with the corresponding shift of the oxyhemoglobin dissociation curve to the left . Those. there is an increase in the affinity of hemoglobin for oxygen, which reduces the flow of the latter into the tissues. In addition, respiratory alkalosis leads to ischemic hypoxia of the brain (spasm of cerebral vessels), as well as to an increase in intravascular capacity (dilatation of somatic arterioles). The result of such dilatation is pathological deposition of blood in the periphery, accompanied by a violation of the systemic (fall in BCC and cardiac output) and organ (impaired microcirculation) blood flow. In this way, exogenous mechanism of hypobaric hypoxic hypoxia, due to a decrease in the partial pressure of oxygen in the inhaled air, will be supplemented endogenous (hemic and circulatory) mechanisms of hypoxia, which will determine the subsequent development of metabolic acidosis(Fig. 6).
Hypoxia is most clearly detected during a stay in a rarefied space, when the partial pressure of oxygen drops.
In an experiment, oxygen starvation can occur at relatively normal atmospheric pressure, but with a reduced oxygen content in the surrounding atmosphere, for example, when an animal stays in a closed space with a reduced oxygen content. The phenomena of oxygen starvation can be observed when climbing mountains, climbing in an airplane to a great height - mountain and altitude sickness(Fig. 116).
The first signs of acute mountain sickness can often be observed already at an altitude of 2500 - 3000 m. In most people, they appear when climbing to 4000 m and above. The partial pressure of oxygen in the air, equal (at atmospheric pressure 760 mm Hg) 159 mm, drops at this height (430 mm atmospheric pressure) to 89 mm. At the same time, arterial oxygen saturation begins to decrease. Symptoms of hypoxia usually appear when arterial oxygen saturation is about 85%, and death can occur when arterial oxygen saturation falls below 50%.
Climbing the mountain is accompanied characteristic phenomena also due to temperature conditions, wind and muscle activity performed during lifting. The more the metabolism increases due to muscle tension or a decrease in air temperature, the sooner the signs of the disease occur.
Disorders that occur during ascent to a height develop the stronger, the faster the ascent is made. Great importance while having training.
Oxygen starvation during ascent in an airplane to a high altitude is distinguished by some features. Climbing a mountain is slow and requires intense muscular work. Planes, on the other hand, can reach altitude in a very short time. The stay of a pilot at an altitude of 5000 m in the absence of sufficient training is accompanied by sensations of headache, dizziness, heaviness in the chest, palpitations, expansion of gases in the intestines, as a result of which the diaphragm is pushed upward, and breathing becomes even more difficult. The use of oxygen devices eliminates many of these phenomena (Fig. 117).

The impact on the body of a low oxygen content in the air is expressed in disorders of the function nervous system, respiration and circulation.
Some excitement is followed by fatigue, apathy, drowsiness, heaviness in the head, mental disorders in the form of irritability followed by depression, some loss of orientation, disorders of motor function, and disorders of higher nervous activity. At medium altitudes, a weakening of internal inhibition develops in the cerebral cortex, and at higher altitudes, diffuse inhibition develops. Disturbances of vegetative functions also develop in the form of shortness of breath, increased heart rate, changes in blood circulation and indigestion.
With an acute onset of oxygen starvation, the breath. It becomes superficial and frequent, which is the result of excitation of the respiratory center. Sometimes there is a peculiar, intermittent, so-called periodic breathing (such as Cheyne-Stokes). At the same time, pulmonary ventilation is noticeably affected. With gradually onset oxygen starvation, breathing becomes frequent and deep, air circulation in the alveoli improves markedly, but the carbon dioxide content and its tension in the alveolar air fall, that is, hypocapnia develops, complicating the course of hypoxia. Respiratory failure can cause loss of consciousness.
Acceleration and intensification of the activity of the heart arise due to an increase in the function of its accelerating and reinforcing nerves, as well as a decrease in the function of the vagus nerves. Therefore, an increase in the pulse during oxygen starvation is one of the indicators of the reaction of the nervous system that regulates blood circulation.
On the high altitude a number of other circulatory disorders also occur. Arterial pressure first rises, but then begins to decrease in accordance with the state of the vasomotor centers. With a sharp decrease in the oxygen content in the inhaled air (up to 7-6%), the activity of the heart noticeably weakens, blood pressure drops, and venous pressure rises, cyanosis and arrhythmia develop.
Sometimes there is also bleeding from the mucous membranes of the nose, mouth, conjunctiva, respiratory tract, gastrointestinal tract. Great importance in the occurrence of such bleeding is attached to the expansion of superficial blood vessels and the violation of their permeability. These changes are partly due to the action of toxic metabolic products on the capillaries.
Violation of the function of the nervous system from staying in a rarefied space also manifests itself disorders of the gastrointestinal tract usually in the form of lack of appetite, inhibition of the activity of the digestive glands, diarrhea and vomiting.
In high-altitude hypoxia, the metabolism. Oxygen consumption initially rises, and then, with pronounced oxygen starvation, falls, the specific dynamic action of the protein decreases, and the nitrogen balance becomes negative. Residual nitrogen in the blood increases, ketone bodies accumulate, especially acetone, which is excreted in the urine.
Reducing the oxygen content in the air to a certain limit has little effect on the formation of oxyhemoglobin. However, in the future, with a decrease in the oxygen content in the air to 12%, the saturation of the blood with oxygen becomes about 75%, and when the content of oxygen in the air is 6–7%, it is 50–35% of normal. The tension of oxygen in the capillary blood is especially reduced, which noticeably affects its diffusion into the tissue.
An increase in pulmonary ventilation and an increase in the respiratory volume of the lungs during hypoxia cause the depletion of alveolar air and blood with carbon dioxide (hypocapnia) and the occurrence of relative alkalosis, as a result of which the excitability of the respiratory center may temporarily be inhibited, and the activity of the heart is weakened. Therefore, the inhalation of carbon dioxide at altitudes, causing an increase in the excitability of the respiratory center, increases the oxygen content in the blood and thereby improves the condition of the body.
However, the continuing decrease in the partial pressure of oxygen during ascent to a height contributes to the further development of hypoxemia and hypoxia. The phenomena of insufficiency of oxidative processes are growing. Alkalosis is again replaced by acidosis, which is again somewhat weakened due to an increase in the rhythm of respiration, a decrease in oxidative processes and a partial pressure of carbon dioxide.
Significantly changed when climbing to a height and heat exchange. Heat transfer at high altitude increases mainly due to the evaporation of water by the surface of the body and through the lungs. Heat production gradually lags behind heat transfer, as a result of which the body temperature, which initially rises slightly, then decreases.
The onset of signs of oxygen starvation largely depends on the characteristics of the organism, the state of its nervous system, lungs, heart and blood vessels, which determine the body's ability to tolerate a rarefied atmosphere.
The nature of the action of rarefied air also depends on the rate of development of oxygen starvation. In acute oxygen starvation, the dysfunction of the nervous system comes to the fore, while in chronic oxygen starvation, due to the gradual development of compensatory processes, pathological phenomena from the nervous system are not detected for a long time.
In general, a healthy person copes satisfactorily with lowering the barometric pressure and the partial pressure of oxygen to a certain limit, and the better, the slower the ascent is made and the more easily the organism adapts. The limit for a person can be considered a decrease in atmospheric pressure to one third of normal, i.e., up to 250 mm Hg. Art., which corresponds to an altitude of 8000 - 8500 m and an oxygen content in the air of 4 - 5%.
It has been established that during a stay at heights, fixture organism, or its acclimatization, providing compensation for respiratory disorders. In mountainous areas and trained climbers, mountain sickness may not develop when climbing to a height of 4000-5000 m. Highly trained pilots can fly without an oxygen apparatus at an altitude of 6000-7000 m and even higher.
Under normal conditions, a person breathes ordinary air, which has a relatively constant composition (Table 1). Exhaled air always contains less oxygen and more carbon dioxide. The least oxygen and the most carbon dioxide in the alveolar air. The difference in the composition of alveolar and exhaled air is explained by the fact that the latter is a mixture of dead space air and alveolar air.
Alveolar air is the internal gas environment of the body. The gas composition of arterial blood depends on its composition. Regulatory mechanisms maintain the constancy of the composition of the alveolar air. The composition of the alveolar air during quiet breathing depends little on the phases of inhalation and exhalation. For example, the content of carbon dioxide at the end of inhalation is only 0.2-0.3% less than at the end of exhalation, since only 1/7 of the alveolar air is renewed with each breath. In addition, it flows continuously, during inhalation and exhalation, which helps to equalize the composition of the alveolar air. With deep breathing, the dependence of the composition of the alveolar air on inhalation and exhalation increases.
Table 1. Composition of air (in %)
Gas exchange in the lungs is carried out as a result of the diffusion of oxygen from the alveolar air into the blood (about 500 liters per day) and carbon dioxide from the blood into the alveolar air (about 430 liters per day). Diffusion occurs due to the difference in the partial pressure of these gases in the alveolar air and their tension in the blood.
Partial gas pressure: concept and formula
Partial pressure gas in a gas mixture in proportion to the percentage of gas and the total pressure of the mixture:
For air: P atmospheric = 760 mm Hg. Art.; With oxygen = 20.95%.
It depends on the nature of the gas. The entire gas mixture of atmospheric air is taken as 100%, it has a pressure of 760 mm Hg. Art., and part of the gas (oxygen - 20.95%) is taken as X. Hence the partial pressure of oxygen in the air mixture is 159 mm Hg. Art. When calculating the partial pressure of gases in the alveolar air, it must be taken into account that it is saturated with water vapor, the pressure of which is 47 mm Hg. Art. Consequently, the share of the gas mixture that is part of the alveolar air has a pressure of not 760 mm Hg. Art., and 760 - 47 \u003d 713 mm Hg. Art. This pressure is taken as 100%. From here it is easy to calculate that the partial pressure of oxygen, which is contained in the alveolar air in the amount of 14.3%, will be equal to 102 mm Hg. Art.; accordingly, the calculation of the partial pressure of carbon dioxide shows that it is equal to 40 mm Hg. Art.
The partial pressure of oxygen and carbon dioxide in the alveolar air is the force with which the molecules of these gases tend to penetrate through the alveolar membrane into the blood.
Diffusion of gases through the barrier obeys Fick's law; since the membrane thickness and diffusion area are the same, diffusion depends on the diffusion coefficient and pressure gradient:
![]()
Q gas- the volume of gas passing through the tissue per unit time; S - tissue area; DK-diffusion coefficient of the gas; (P 1, - P 2) - gas partial pressure gradient; T is the thickness of the tissue barrier.
If we take into account that in the alveolar blood flowing to the lungs, the partial oxygen tension is 40 mm Hg. Art., and carbon dioxide - 46-48 mm Hg. Art., then the pressure gradient that determines the diffusion of gases in the lungs will be: for oxygen 102 - 40 = 62 mm Hg. Art.; for carbon dioxide 40 - 46 (48) \u003d minus 6 - minus 8 mm Hg. Art. Since the diffuse coefficient of carbon dioxide is 25 times greater than that of oxygen, carbon dioxide leaves the capillaries more actively into the alveoli than oxygen in the opposite direction.
In the blood, gases are in a dissolved (free) and chemically bound state. Diffusion involves only dissolved gas molecules. The amount of gas that dissolves in a liquid depends on:
- on the composition of the liquid;
- volume and pressure of gas in liquid;
- liquid temperature;
- the nature of the gas under study.
The higher the pressure of a given gas and the temperature, the more the gas dissolves in the liquid. At a pressure of 760 mm Hg. Art. and a temperature of 38 ° C, 2.2% oxygen and 5.1% carbon dioxide dissolve in 1 ml of blood.
The dissolution of a gas in a liquid continues until a dynamic equilibrium is reached between the number of gas molecules dissolving and escaping into the gaseous medium. The force with which the molecules of a dissolved gas tend to escape into a gaseous medium is called pressure of a gas in a liquid. Thus, at equilibrium, the gas pressure is equal to the partial pressure of the gas in the liquid.
If the partial pressure of a gas is higher than its voltage, then the gas will dissolve. If the partial pressure of the gas is below its voltage, then the gas will go out of solution into the gaseous medium.
The partial pressure and tension of oxygen and carbon dioxide in the lungs are given in Table. 2.
Table 2. Partial pressure and tension of oxygen and carbon dioxide in the lungs (in mmHg)
Diffusion of oxygen is provided by the difference in partial pressures in the alveoli and blood, which is equal to 62 mm Hg. Art., and for carbon dioxide - it is only about 6 mm Hg. Art. The time of blood flow through the capillaries of the small circle (an average of 0.7 s) is sufficient for almost complete equalization of partial pressure and gas tension: oxygen dissolves in the blood, and carbon dioxide passes into the alveolar air. The transition of carbon dioxide into alveolar air at a relatively small pressure difference is explained by the high diffusion capacity of the lungs for this gas.
If there is a mixture of gases above the liquid, then each gas dissolves in it according to its partial pressure, in the mixture, i.e., to the pressure that falls on its share. Partial pressure of any gas in a gas mixture can be calculated by knowing the total pressure of the gas mixture and its percentage composition. So, at atmospheric air pressure of 700 mm Hg. the partial pressure of oxygen is approximately 21% of 760 mm, i.e. 159 mm, nitrogen - 79% of 700 mm, i.e. 601 mm.
When calculating partial pressure of gases in the alveolar air, it should be taken into account that it is saturated with water vapor, the partial pressure of which at body temperature is 47 mm Hg. Art. Therefore, the share of other gases (nitrogen, oxygen, carbon dioxide) is no longer 700 mm, but 700-47 - 713 mm. With an oxygen content in the alveolar air equal to 14.3%, its partial pressure will be only 102 mm; with a carbon dioxide content of 5.6%, its partial pressure is 40 mm.
If a liquid saturated with a gas at a certain partial pressure comes into contact with the same gas, but having a lower pressure, then part of the gas will come out of solution and the amount of dissolved gas will decrease. If the gas pressure is higher, then more gas will dissolve in the liquid.
The dissolution of gases depends on the partial pressure, i.e., the pressure of a particular gas, and not the total pressure of the gas mixture. Therefore, for example, oxygen dissolved in a liquid will escape into a nitrogen atmosphere in the same way as into a void, even when the nitrogen is under very high pressure.
When a liquid comes into contact with a gas mixture of a certain composition, the amount of gas that enters or leaves the liquid depends not only on the ratio of gas pressures in the liquid and in the gas mixture, but also on their volumes. If a large volume of liquid is in contact with a large volume of a gas mixture whose pressure differs sharply from the pressure of the gases in the liquid, then large quantities of gas may escape or enter into the latter. On the contrary, if a sufficiently large volume of liquid comes into contact with a gas bubble of small volume, then a very small amount of gas will leave or enter the liquid, and the gas composition of the liquid will practically not change.
For gases dissolved in a liquid, the term " voltage”, corresponding to the term “partial pressure” for free gases. Voltage is expressed in the same units as pressure, i.e. in atmospheres or in millimeters of mercury or water column. If the gas pressure is 1.00 mm Hg. Art., this means that the gas dissolved in the liquid is in equilibrium with the free gas under pressure of 100 mm.
If the tension of the dissolved gas is not equal to the partial pressure of the free gas, then the equilibrium is disturbed. It is restored when these two quantities again become equal to each other. For example, if the oxygen pressure in the liquid of a closed vessel is 100 mm, and the oxygen pressure in the air of this vessel is 150 mm, then oxygen will enter the liquid.
In this case, the tension of oxygen in the liquid will be dismissed, and its pressure outside the liquid will decrease until a new dynamic equilibrium is established and both of these values are equal, having received some new value between 150 and 100 mm. How the pressure and stress change in a given study depends on the relative volumes of gas and liquid.
PaO2, along with two other quantities (paCO2 and pH), make up such a concept as "blood gases" (Arterial blood gases - ABG (s)). The value of paO2 depends on many parameters, the main of which are the age and height of the patient (partial pressure of O2 in atmospheric air). Thus, pO2 must be interpreted individually for each patient.
Accurate results for ABGs depend on the collection, processing, and actual analysis of the sample. Clinically important errors can occur at any of these steps, but blood gas measurements are particularly vulnerable to errors that occur prior to analysis. The most common problems include
- sampling of non-arterial (mixed or venous) blood;
- the presence of air bubbles in the sample;
- insufficient or excessive amount of anticoagulant in the sample;
- delaying the analysis and keeping the sample uncooled all this time.
A proper blood sample for ABG analysis typically contains 1-3 ml of arterial blood drawn anaerobically from a peripheral artery into a special plastic container using a small diameter needle. Air bubbles that may enter during sampling must be removed immediately. The air in the room has a paO2 of about 150 mmHg. (at sea level) and paCO2 is practically equal to zero. Thus, air bubbles that mix with arterial blood shift (increase) paO2 to 150 mm Hg. and reduce (decrease) paCO2.
If heparin is used as an anticoagulant and the sampling is done with a syringe and not with a special container, the pH of heparin, which is approximately 7.0, should be taken into account. Thus, an excess of heparin can change all three ABG values (paO2, paCO2, pH). A very small amount of heparin is needed to prevent clotting; 0.05 - 0.10 ml of a dilute solution of heparin (1000 IU / ml) will counteract the clotting of approximately 1 ml of blood without affecting pH, paO2, paCO2. After flushing the syringe with heparin, a sufficient amount of heparin usually remains in the dead space of the syringe and needle, which is enough to anticoagulate without distorting the ABG values.
After collection, the sample should be analyzed as soon as possible. If a delay of more than 10 minutes occurs, the sample must be immersed in a container with ice. Leukocytes and platelets continue to consume oxygen in the sample after collection, and can cause a significant drop in paO2 when stored for long periods at room temperature, especially under conditions of leukocytosis or thrombocytosis. Cooling will prevent any clinically important changes for at least 1 hour by reducing the metabolic activity of these cells.